Everyone should have equal access to the full range of end-of-life care options. Compassion & Choices is working in partnership with our Leadership Councils and partner organizations to address inequities in end-of-life care and planning.
Our mission is to improve care, expand options and empower everybody to understand their options so they can have an end-of-life experience that is consistent with their values and priorities. Racially and ethnically diverse communities, LGBTQ+ communities, and those with disabilities face systemic and persistent inequities in end-of-life healthcare that mean they are less likely to have the information necessary to be fully empowered to have a death consistent with their values and priorities. To achieve our mission, we work in partnership with the impacted communities to address these inequities including changing laws, the health system and empowering communities with information.
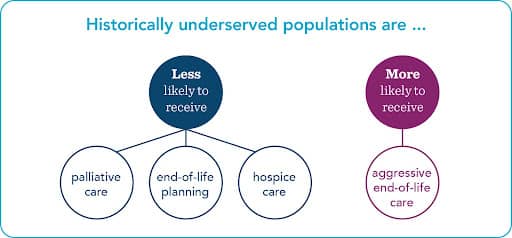
Data indicates that historically underserved communities are less like to have meaningful information about and access to:
And more likely to receive aggressive end-of-life care that does not increase, and may reduce, quality of life.1 Individuals with different beliefs may choose different levels of care. However, those preferences should come as a result of fully informed decision making, not as a result of systemic inequities in the healthcare system that results in lack of awareness and access to available options. See figure below as well as these data slides.
A Compassion & Choices research scan of published articles between 2018 and 2021 confirms that end-of-life inequities exist at least for the following populations:
Note that inequities may also exist among other communities.
Inequities that historically underserved communities face at the end-of-life are a continuation of the inequities faced throughout their life. The figure below outlines some of the most common factors driving disparities–one factor or all of them together may lead to inequities in end-of-life planning and care. As an example:


Addressing inequities in end-of-life care will not happen overnight, however, the summit report produced by Compassion & Choices and our partner organizations includes a comprehensive review of potential actions that can be taken to address these inequities. Below is a highlight:
1 https://www.liebertpub.com/doi/abs/10.1089/jpm.2018.0436; ; https://www.sciencedirect.com/science/article/pii/S0885392418300277#bib6.
2 https://pubmed.ncbi.nlm.nih.gov/32767722/; https://onlinelibrary.wiley.com/doi/full/10.1002/hast.1135; https://proceedings.med.ucla.edu/wp-content/uploads/2020/06/Wells-A200421LW-rko-Wells-Lindsay-M.D.-BLM-formatted.pdf.
4 Cindy L. Cain, et al., Culture and Palliative Care: Preferences, Communication, Meaning, and Mutual Decision Making, 55(5) J Pain Symptom and Management 1408-1419 (2018) https://www.sciencedirect.com/science/article/pii/S0885392418300277#bib6
5 Cindy L. Cain, et al., Culture and Palliative Care: Preferences, Communication, Meaning, and Mutual Decision Making, 55(5) J Pain Symptom and Management 1408-1419 (2018) https://www.sciencedirect.com/science/article/pii/S0885392418300277#bib6
Mail contributions directly to:
Compassion & Choices Gift Processing Center
PO Box 485
Etna, NH 03750