Part I: Growth of Religiously-Affiliated Healthcare Institutions: Why it Matters
Oct 28, 2020 Kim Callinan author

This is the first of a two-part series: Growth of Religiously-Affiliated Healthcare Institutions. Read Part II: Our Path Forward.
Chris was just 29 years old when he faced the late stages of bladder cancer — which was ravaging his body. He had talked with his wife, Amanda, well before this last stage of the disease, of his desire to use medical aid in dying if his suffering became unbearable. Medical aid in dying would allow Chris to request a prescription he could decide to take to die peacefully in his sleep.
Despite California’s law allowing medical aid in dying, Chris was unable to locate a physician in his health system willing to prescribe him the needed medication. He ultimately suffered greatly in his last days.
Chris was receiving his care in a religiously-affiliated hospital that forbids physicians from complying with an aid-in-dying request. The care Chris and others like him receive in such healthcare facilities is often of high quality and compassionate; yet, limiting care choices for patients without their knowledge or consent is nothing short of unconscionable. Some Adventist facilities, such as Chris’, and all Catholic healthcare facilities restrict the practice of medical aid in dying.
Catholic facilities in particular are governed by strict standards, Ethical and Religious Directives for Catholic Health Care Services (ERDs), which are issued and enforced by the U.S. Conference of Catholic Bishops.
Earlier this month, Community Catalyst published a report, Bigger and Bigger: The Growth of Catholic Health Systems. It noted that the number of Catholic-affiliated hospitals grew by more than 28% over the last two decades, even as the number of secular hospitals dropped by nearly 14%. That means, faced with a serious or terminal illness, we have a good chance of receiving our care in one of these facilities.
The Growth of Religiously-Based Healthcare Facilities and Why it Matters
Why does it matter whether we receive our end-of-life care from a religiously-affiliated healthcare system? Here’s what’s in jeopardy:
- Full transparency and the right to know. Patients must have full and clear information about the healthcare facility they choose to use: transparency for prescription drugs, healthcare services, and policies governing what services are covered and offered by a provider. Withholding information about healthcare services or options, such as medical aid in dying, violates both legal and ethical obligations. Chris and his wife were unaware that the facility where he was receiving care forbade their physicians from practicing medical aid dying. He was denied the right to make an informed decision about what healthcare he would receive.
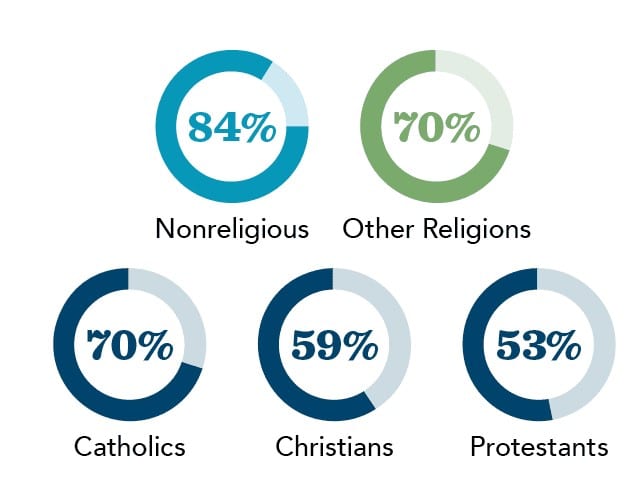
- Individual rights to care that align with our values/preferences. Many religiously-based healthcare systems are governed by directives that forbid physicians from offering patients the full range of legal end-of-life options. Medical aid in dying is one of those options. The majority of Americans of all religions support medical aid in dying (see infographic below). It’s the institutional policies of religiously-based systems that oppose the option and block access. Patients rights should not be secondary to the rights of institutions.
Medical aid in dying is already voluntary. No healthcare provider is obligated to prescribe or consult in such cases. However, regardless of a provider’s own personal or institutional beliefs, there exists a professional responsibility to provide the patient with information and referrals for medical aid in dying or to even transfer a patient’s medical record to a provider of the patient's choice.
- Competition and free markets. Mergers and consolidations increasingly have decreased consumer and patient options to access care that meets their individual needs. This includes access to the full range of end-of-life care options including medical aid in dying, the withdrawal of treatment and even palliative sedation.
- Access for underserved communities where there are few or no safety net providers. The Community Catalyst report found that in five states (Alaska, Iowa, South Dakota, Washington and Wisconsin) over 40% of all acute care beds are in Catholic hospitals. Fifty-two hospitals are designated as the sole community hospital (at least 35 miles away from another hospital) in their region, an increase from 30 in 2013. That means, many people residing in rural areas, for example, may not have any other options for care.
In recent years, we’ve seen court cases come before the U.S. Supreme Court that expand who qualifies for protections under the first amendment and what constitutes participation. In Little Sisters of the Poor v. Pennsylvania, the court ruled that the federal administrative rules around the Affordable Care Act were constitutional. These rules allow employers to deny benefits, like contraception, mandated in the Affordable Care Act if they are religiously or morally opposed to them, and to do so without notifying the government or the patient. The decision also reinforced earlier Supreme Court rulings (Hobby Lobby, Zubik) which expanded religious protections from churches to any commercial entity seeking to impose their moral agendas on employees.
The growth of such religiously-based institutions is disconcerting at best and quite damaging to our individual rights at their fullest potential.
Next Up: Part II: Our Path Forward


