Compassion & Choices is leading efforts to authorize, implement and defend medical aid in dying so all terminally ill people who are eligible will have access to the full range of end-of-life care options.
Why does Compassion & Choices focus on authorizing and implementing medical aid in dying?
Medical aid in dying is a widely supported end-of-life option that provides dying people with peace of mind and comfort during a difficult time. While only a small number of people will choose to use the option, to patients, it is a prime litmus test of person-directed care. It exemplifies a medical system that respects patients by allowing them to assert their values and priorities as death approaches. Furthermore, the evidence demonstrates that authorizing medical aid in dying protects patients, affords dying people autonomy and compassion during the most difficult time, improves end-of-life care even for those who don’t choose the option, and costs states almost nothing to implement.
What is medical aid in dying?
A trusted and time-tested medical practice that allows a terminally ill, mentally capable adult with a prognosis of six months or less to live to request from their doctor a prescription for medication they can decide to self-ingest to die peacefully in their sleep.
Medical aid in dying is sometimes incorrectly referred to as “assisted physician suicide,” “physician aid in dying,” “death with dignity,” and “euthanasia.” Medical aid in dying is not assisted suicide, suicide, or euthanasia. These terms are misleading and factually incorrect.
Where is medical aid in dying authorized?
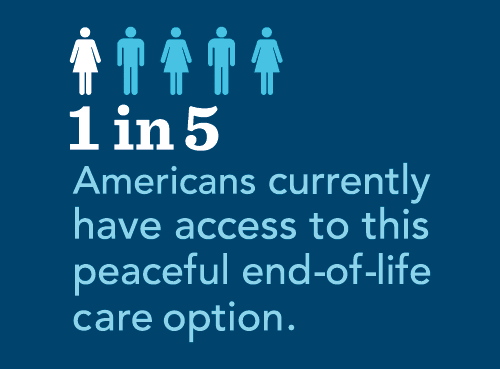
Compassion & Choices has led or supported campaigns to authorize medical aid in dying and implement this medical practice in 11 jurisdictions, giving one in five Americans the end-of-life option (dates indicate when the law was enacted):
- California End of Life Option Act, 2015 (legislation) Reauthorized in 2021 (legislation)
- Colorado End-of-Life Options Act, 2016 (ballot initiative)
- District of Columbia Death with Dignity Act, 2017 (legislation)
- Hawai‘i Our Care, Our Choice Act, 2018 (legislation)
- Maine Death with Dignity Act, 2019 (legislation)
- Montana, 2009 (Supreme Court ruling)
- New Jersey Aid in Dying for the Terminally Ill Act, 2019 (legislation)
- New Mexico Elizabeth Whitefield End-of-Life Options Act, 2021 (legislation)
- Oregon Death with Dignity Act, 1997 (ballot initiative)
- Vermont Patient Choice and Control at the End of Life Act, 2013 (legislation)
- Washington Death with Dignity Act, 2008 (ballot initiative)
See a chart listing the jurisdictions in order of they were authorized.
Is medical aid in dying safe?
With more than 20 years of evidence from Oregon alone and another 20 years of combined evidence in the other authorized jurisdictions, the laws that authorize this compassionate option have proven not only to protect patients, but to improve care across the end-of-life spectrum. The fundamental core safeguards embedded in medical aid-in-dying laws ensure that all terminally ill individuals pursuing the option are protected from coercion and abuse.
After watching my husband John suffer terribly at the end of his life, I strongly believe in our right to choose when we die, if our illness is beyond any hope of meaningful recovery.” -- Diane Rehm, NPR host of the Diane Rehm Show
Medical aid in dying protects patients, affords dying people autonomy and compassion during the most difficult time, improves end-of-life care, and costs states almost nothing to implement, except for the minimal costs associated with collecting data and producing the annual statistical reports.
Who is eligible for medical aid in dying?

"I support medical aid and dying because I think it will give so many terminal patients some sense of control when pain becomes unbearable." —Fay Hoh Yin
To be eligible for aid-in-dying medication, an individual must meet all four criteria:
- An adult (aged 18 or older);
- Terminally ill with a prognosis of six months or less to live;
- Mentally capable of making their own healthcare decisions; and
- Able to self-ingest the medication.
What safeguards are in place?
In addition to the strict eligibility criteria these laws establish the following core safeguards:
- The attending physician must inform the terminally ill adult requesting medical aid in dying about all other end-of-life care options. These other options include comfort care, hospice care, pain control and palliative care;
- The attending physician must inform the terminally ill adult requesting medical aid in dying that they can change their mind at any time. This patient right to change their mind includes deciding not to self-ingest the medication once they have obtained it;
- The attending physician must also offer the individual an opportunity to rescind their request.
These core safeguards ensure that individual patient preferences, needs and values are honored, and guide all clinical decisions, including the decision to use medical aid in dying.
How does medical aid in dying benefit society?
Society benefits when medical aid in dying laws are implemented -- benefits that help everybody -- regardless of whether one decides to access the law:
- Improved conversations between doctors and patients
- Better use of hospice
- Better physician training in end-of-life care
Who supports medical aid in dying?
Three quarters of Americans (74%) support the option of medical aid in dying, according to the 2020 Gallup Poll. Support is high across all demographic groups surveyed. Read more about support for medical aid in dying in the latest polls.
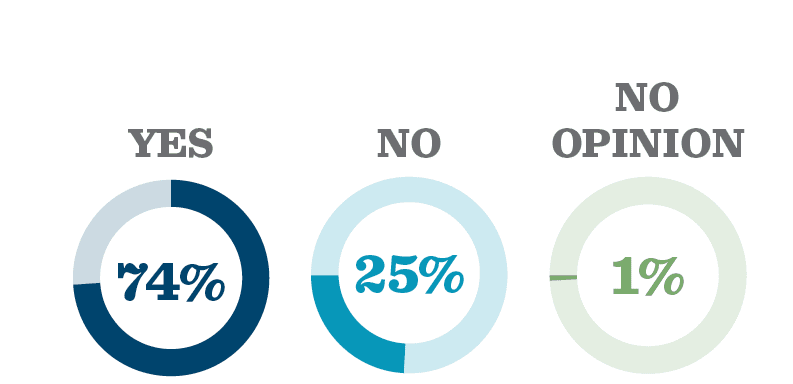
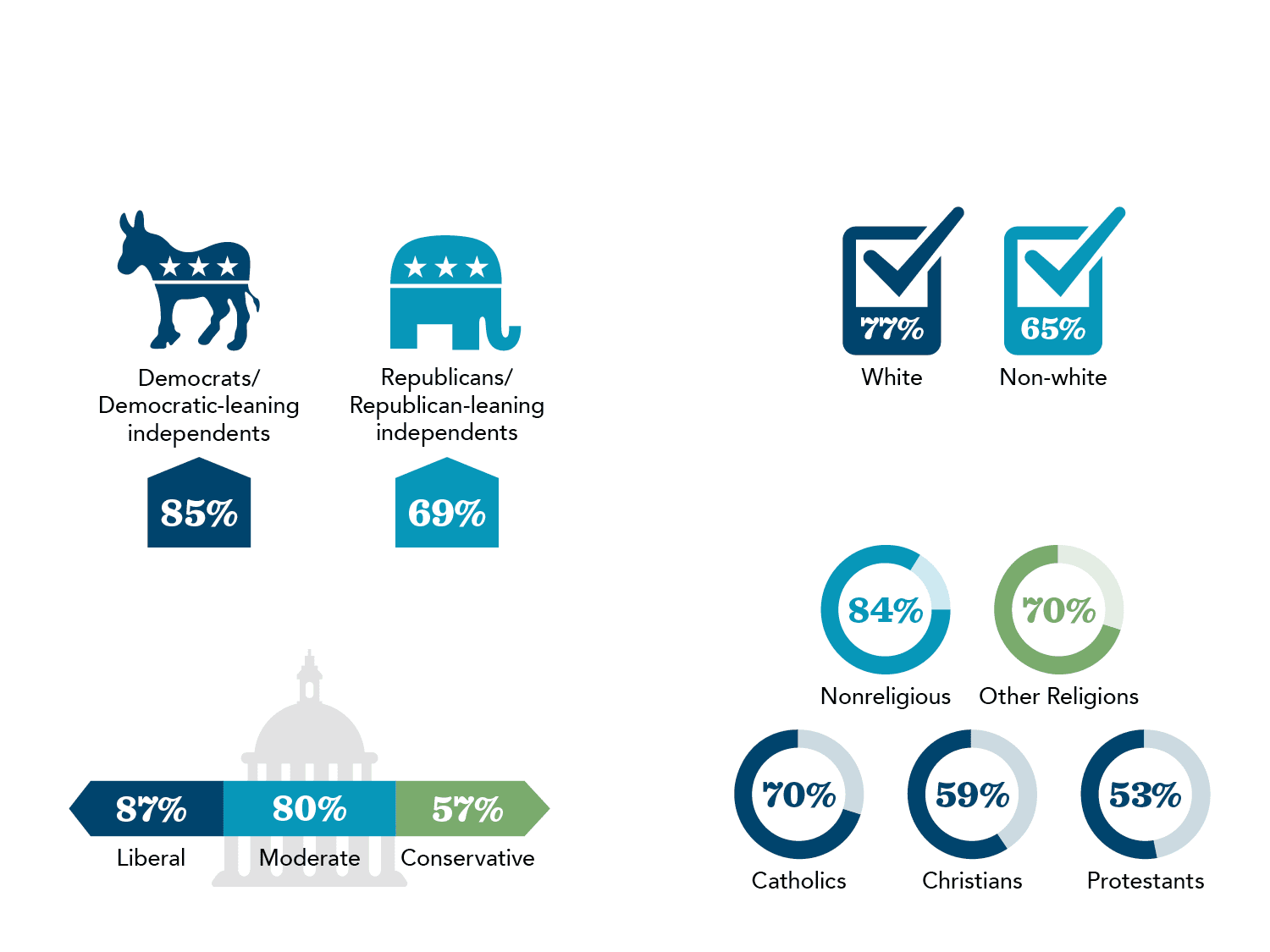
Source: Gallup Poll, 2020.
Resources
If you don't see what you are looking for, visit our Resources page.
The Basics
- FAQs Medical aid in dying FAQs
- Facts About Medical Aid in Dying
- Insurance Coverage and Medical Aid in Dying
- Medical Aid in Dying & People with Disabilities
- Medical Aid in Dying and Palliative Care
- Medical Aid in Dying Is Not Suicide
- Prognosis to Prescription
- Glossary of Terms
Volunteer Action Network
Policy/Legal/Advocacy
- Medical Aid in Dying Policy Book
- Americans Support Medical Aid in Dying
- Polling Support for Medical Aid in Dying
- Faith Communities & Leaders Support Medical Aid in Dying
- FAQs for Faith Leaders
- Medical Associations and Medical Aid in Dying
- Laws Work to Protect Patients
- Statutory Waiting Period Chart
State End-of-Life Information Packets
State-specific booklets that provide step-by-step instructions for how to use the law, how to find a physician and what to consider when talking with your physician. Also see the Medical Aid in Dying tracking sheet
- California
- Colorado
- Hawai‘i
- District of Columbia
- Montana
- New Jersey
- New Mexico
- Oregon
- Vermont
- Washington
Webinars
Medical Aid in Dying and ALS: How the Option Can End Suffering
How Medical Aid in Dying Really Works in Authorized States
Patient Perspective on Medical Aid in Dying
Medical Aid in Dying: Ensuring Access to the End of Life Option that you Want


