Lindsay and Stephanie shared their story in January of 2021.
Erik Carlson was first diagnosed with glioblastoma, the most aggressive, incurable brain cancer, in the spring of 2019, after tingling in his left arm led him to seek medical attention. Erik was not the type to visit a doctor unnecessarily. As an extremely active outdoorsman with a high pain threshold, his hand would need to be hanging on by a thread for him to see a physician. When the tingling turned into numbness in his arm while driving, it scared him enough to pull over on the side of the road. He realized this wasn't something he should ignore.
The doctor ordered an MRI, then another, but this time with contrast. Erik and Stephanie did not expect any significant news. Erik was young, had never experienced any significant health issues, and was active every single day of his life. There was no reason to feel concerned.
The next day, Erik called Stephanie to share that the doctor had just called. Erik had a brain tumor and would need to see the neurosurgeon the following day. How could this be? He was healthy, and aside from the little bit of tingling, there were zero outward signs of cancer.
The following day, the neurosurgeon said it didn’t look good. Surgery was scheduled for the next morning. Shocked by the news, Erik and Stephanie sat in the medical center parking lot and started making calls to family and close friends. Lindsay, Erik’s sister, booked the first available flight from Colorado to join her brother in Maine.
In a way, the immediate response necessitated by the situation served as a blessing. There was no time to sit in fear and worry about what could happen. It was the best of a terrible situation, as Erik would continue to say throughout the next 18 months.
While Erik endured brain surgery, Stephanie, Lindsay, Erik’s daughters Isabel and Amelia and other close loved ones sat in the waiting room desperate for good news.
After the surgery, they were all relieved that Erik was recovering and that the neurosurgeon had been able to remove the majority of the cancer cells. The surgeon, however, did not waste any time in bringing everyone back to the reality that Erik was facing a bad situation: “This will kill him. Erik is too young and too healthy for something different to kill him.”
With glioblastoma, the cancer is never gone. It’s not a matter of if someone will die from it, but when.
As Erik remained in the hospital for recovery, he struggled. He hated being inside. Though he had only spent four days in the hospital, to Erik it was an eternity. There wasn’t a day in his 49 years that he did not enjoy the outdoors. Breathing fresh air and being outside was fundamental to his existence. His connection to nature was exceptional – even spiritual. He did not belong confined inside a hospital; and the family had to demand that Erik be allowed a few minutes outside to experience the tranquility he needed.
Upon returning home, Erik was determined to get back to baseline. Within days, he was out on his boat. He was doing the things that helped him – and all of the family – feel normal, while the diagnosis remained unchanged.
Erik’s surgery, and the chemo and radiation that followed, were successful – though not without some challenging side effects. Erik had 14 good months to enjoy with his loved ones, and he took complete advantage of his remaining time.
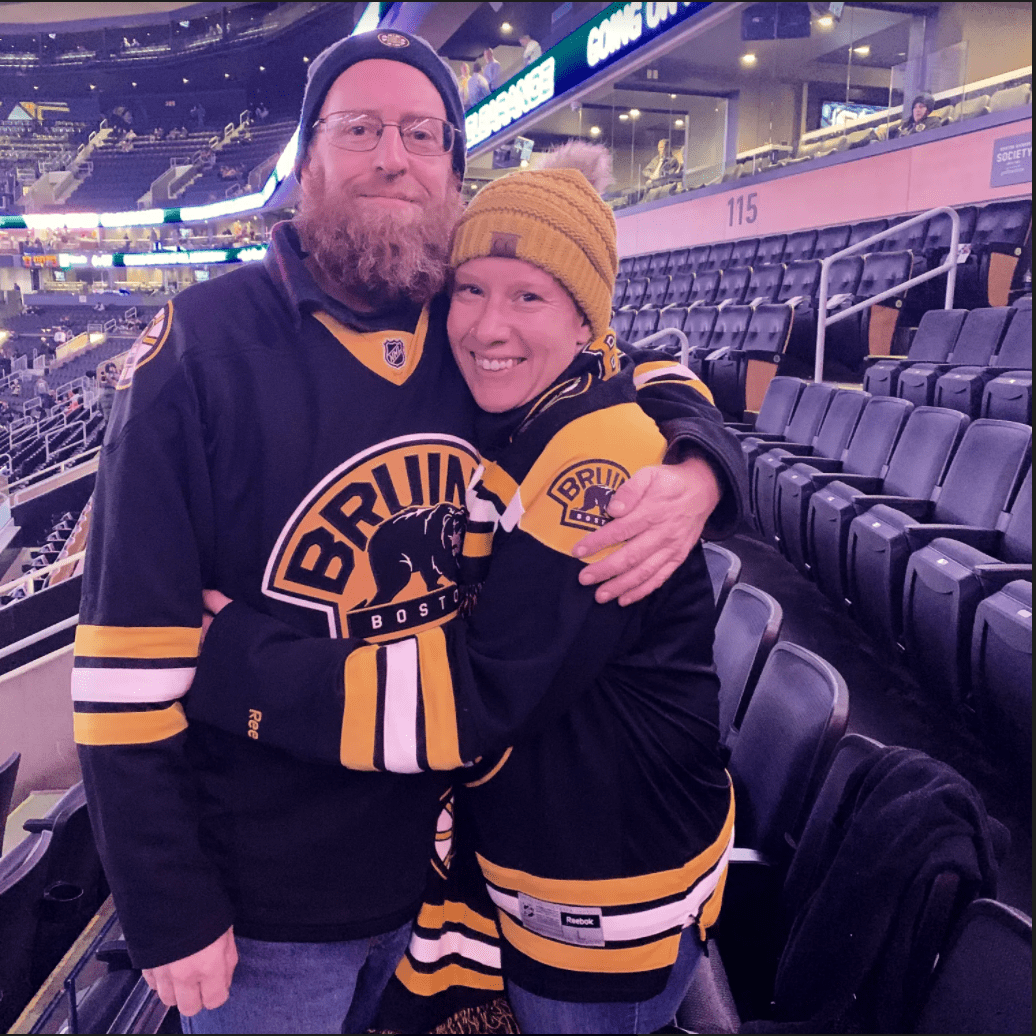
Erik, who was very proud of his Swedish heritage and Viking culture, travelled to Sweden with his daughters to meet relatives and visit an old family farm. He travelled with Stephanie to a secluded island; visited Lindsay and her family in Colorado for Thanksgiving; and went hunting with friends and his beloved canine sidekick, Sula Danger, who was always at his side.
Every six to eight weeks, the family suffered from “scanxiety” – the elevated anxiety they endured due to the fear that the MRI scans to monitor Erik’s cancer would show the tumor had returned. The MRIs were torture for Erik. They represented the hideousness of his reality. The COVID-19 pandemic further exacerbated this because no one could be with him during the MRI.
Things remained stable until the summer of 2020, when Erik suffered a seizure. It scared his daughters and resulted in an emergency room visit. That was the beginning of the end.
Erik was released from the hospital. The follow-up MRI still revealed no tumor, but because of the seizure, Erik’s driver’s license was suspended. Erik was fiercely independent. The near impossibility of living in the woods of Maine without a driver’s license, and the freedom that vanished along with his license was devastating to Erik. No longer could he operate his forestry and logging machinery, escape to the ocean on his boat, or drive himself around even for necessities.
It became evident that Lindsay and Stephanie would need to help Erik maintain as much of his independence as possible to keep his spirits from dipping too low.
An MRI scan in mid-September made it clear that the tumor was back. Erik asked his neuro-oncologist what exactly would happen as he died of glioblastoma. She said Erik would grow increasingly agitated and likely be confined to a wheelchair.
After Erik’s first surgery, he had asked his neuro-oncologist for information about medical aid in dying. Legislation had just passed in Maine, and the idea that this could be an option was comforting. This time, Erik was asking for confirmation that his doctor would sign off if he wanted to access the law.
Determined to fight, Erik planned to endure another surgery to remove the tumor. He was expected to tolerate a second surgery well and hopefully gain another good year. COVID-19 once again complicated Erik’s care. Instead of surgery being scheduled for the following day, it was scheduled two weeks out on October 2. There was time to sit in the fear and obsess over what could go wrong.
Erik went through surgery and suffered unmanageable pain afterwards. Knowing Erik never complained of pain, Stephanie and Lindsay were seriously concerned about his condition and advocated for better pain management. While Erik’s pain remained high, he was released the following day.
Within a day of returning home, he fell to the ground vomiting from the unbearable pain. The pressure of lurching forward and vomiting was dangerous for the brain, and Erik was rushed to the ER. After two days in the hospital, and his pain better under control, Erik returned home.
It quickly became clear that the path forward would be much more difficult than anyone had expected. Erik did not bounce back the way he had from the first surgery. He spent many restless hours, still unable to focus on the things that truly mattered to him.
Ten days after the second surgery, Erik texted Lindsay and Stephanie. He had decided it was time to get an aid-in-dying prescription. He knew he had to make the decision quickly. If he lost his mental capacity, his window of opportunity would close. He wanted to start the process right away.
Stephanie called Erik’s neuro-oncologist to schedule an appointment to request medical aid in dying. With an appointment already scheduled for the following week, his doctor recommended they wait until then. Stephanie responded with an emphatic “No.”
His doctor immediately referred Erik to a local palliative care doctor who had experience with medical aid in dying and was willing to prescribe. Erik’s neuro-oncologist would serve a supportive role as the secondary, consulting doctor.
Lacking the details of the law, Erik expected to receive his prescription by the end of the week. At the visit with the palliative care doctor, it became clear that this would take longer than expected. Erik and Stephanie had forgotten there was a 15-day waiting period, a safeguard that now felt overly burdensome and unnecessary.
After his visit, Erik enlisted the help of hospice, who were wonderful at mitigating his pain and supporting Erik and his family.
The week after Erik’s first request for aid in dying, he realized he wanted to pay it forward and share his story publicly to increase awareness of this meaningful law and the peace of mind it now provided. The previous year, he had emailed Cindy Williams, a local news anchor with NEWS CENTER Maine, to thank her for her very vocal support while the bill was being debated. Now, Erik reached out to offer his personal story to put a face to the legislation and offer an intimate perspective on its significance.
By telling his story, he hoped to help others with terminal illnesses to understand that they had options – some measure of control in an otherwise beyond-control situation. The story subsequently aired after his passing, and many people reached out to thank Erik for his incredible courage. Many in Maine did not know this law existed.
The second week of the waiting period was increasingly difficult for Erik and a detriment to his well-being. There was a psychological burden of having to wait while knowing exactly what he wanted, “I have never been at more peace with a decision in my life, Erik said after making his decision.” However, the wait robbed Erik of being able to keep the joy of living every moment to the fullest.
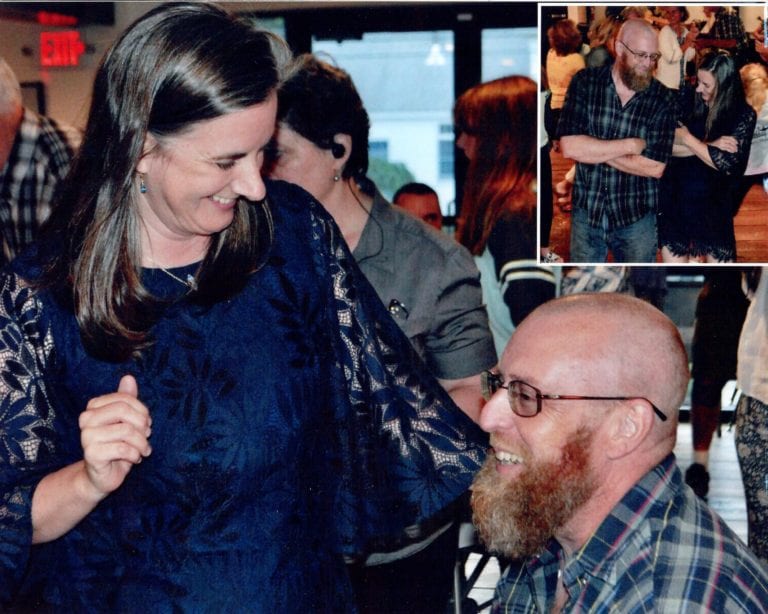
Erik made the most of his 50th birthday, which was October 29, 2020. With his closest friends and relatives there to celebrate his life, Stephanie got the news that Erik’s aid-in-dying prescription was ready for pick up. This information brought a real sense of peace to Erik. He was done “kicking the can down the road,” and was ready for his suffering to cease. To Erik, it was a perfect end to his birthday.
Though Erik’s palliative care doctor could not be present that night, hospice staff were there along with loved ones. His palliative care doctor would remain available for guidance over the phone.
Erik’s last hours were beautiful. His loved ones gathered at the house. It was dark with a huge fire roaring in Erik’s masonry fireplace. There was talking and laughter, with the Rolling Stones playing in the background. Stephanie thought, “You know what, I want to go out like this.”
There was no rush. Everyone was taking their cues from Erik. Lindsay reflected, “This isn’t horrific or depressing. It’s such a gift that Erik is leaving this world as Erik, not as a shell of himself. Losing someone does not have to be shrouded in a black cloud.”
Seventeen days after his first appointment to officially request aid in dying, Erik died at home, as he hoped he would. Through all of it, Erik remained Erik until his last day. Medical aid in dying did not eliminate the grief associated with his death, but in the midst of that grief the fact that Erik was able to take back control eased the sorrow.
Erik was deeply devoted to the people in his life. So many people reached out after his death to share, “I lost my best friend.” He was a truly special human being.
Both Lindsay and Stephanie promised Erik to keep his legacy alive by sharing his experience and the peace of mind this legislation provided him and those he loved. The experience left both women feeling that this option must be made available to anyone in this nation facing a terminal diagnosis.