Everyone should have equal access to the full range of end-of-life care options. Compassion & Choices is working in partnership with our Leadership Councils and partner organizations to address inequities in end-of-life care and planning.
Why Is Compassion & Choices Focused on End-of-Life Inequities?
Our mission is to improve care, expand options and empower everybody to understand their options so they can have an end-of-life experience that is consistent with their values and priorities. Racially and ethnically diverse communities, LGBTQ+ communities, and those with disabilities face systemic and persistent inequities in end-of-life healthcare that mean they are less likely to have the information necessary to be fully empowered to have a death consistent with their values and priorities. To achieve our mission, we work in partnership with the impacted communities to address these inequities including changing laws, the health system and empowering communities with information.
What are Examples of End-of-Life Inequities?
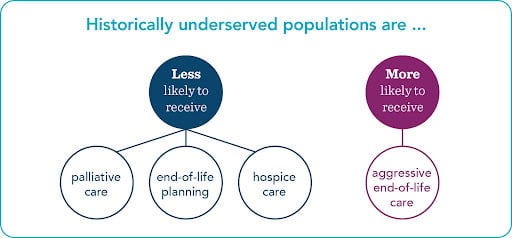
Data indicates that historically underserved communities are less like to have meaningful information about and access to:
- advance care planning
- palliative care
- pain management and
- hospice care.
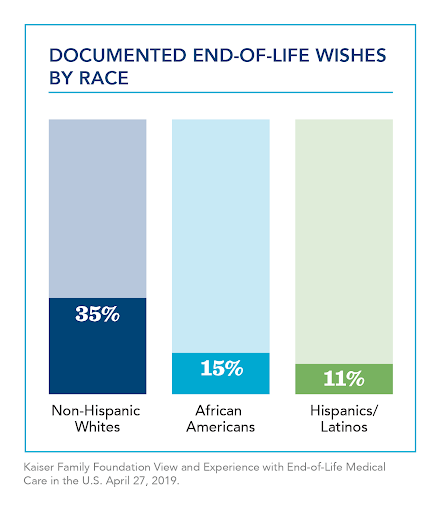
And more likely to receive aggressive end-of-life care that does not increase, and may reduce, quality of life.1 Individuals with different beliefs may choose different levels of care. However, those preferences should come as a result of fully informed decision making, not as a result of systemic inequities in the healthcare system that results in lack of awareness and access to available options. See figure below as well as these data slides.
Which communities are most impacted by end-of-life inequities?
A Compassion & Choices research scan of published articles between 2018 and 2021 confirms that end-of-life inequities exist at least for the following populations:
- Black Americans and African Americans
- Hispanics/Latinos/Latinx
- Asian American, Native Hawaiian and Other Pacific Islanders
- American Indians/Native Americans
- LGBTQ+
Note that inequities may also exist among other communities.
What Causes Inequities in End-of-Life Planning and Care?
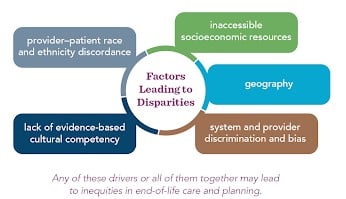
 Inequities that historically underserved communities face at the end-of-life are a continuation of the inequities faced throughout their life. The figure below outlines some of the most common factors driving disparities–one
factor or all of them together may lead to inequities in end-of-life planning and care. As an example:
Inequities that historically underserved communities face at the end-of-life are a continuation of the inequities faced throughout their life. The figure below outlines some of the most common factors driving disparities–one
factor or all of them together may lead to inequities in end-of-life planning and care. As an example:
- Research identifies patient distrust in the healthcare system based on a lifetime of experience with provider bias, discrimination, and hindered access, contributing to inequities in end-of-life care.2
- There is a lack of culturally-competent communication (including communication in a patient’s preferred language) – or sometimes any communication – about end-of-life issues with patients and their loved ones.
What Can Be Done to Address Inequities in End-of-Life Planning and Care?
Addressing inequities in end-of-life care will not happen overnight, however, the summit report produced by Compassion & Choices and our partner organizations includes a comprehensive review of potential actions that can be taken to address these inequities. Below is a highlight:
- Inform and empower all communities’ awareness of the full breadth of legal end-of-life care options as well as the importance of advance care planning so that they make informed care decisions. This includes:
- Starting end-of-life care conversations with patients and their loved ones earlier, before a time of crisis, expecting repeated discussions over time.
- Increase provider and staff education and training on end of life planning and care including helping to build skills on:
- how to recognize and interrupt implicit bias,3
- increasing one’s understanding of patient communication needs including the meaning of suffering for a patient,4 and
- the cultural implications of decision making.5
- Develop more high-quality intervention studies that address racial and ethnic-related health disparities in palliative care.6
- Increase efforts to recruit and retain diverse candidates into medical and nursing schools and other supportive practitioner programs.
Tools and Resources
Tools
- Addressing Inequities in End-of-Life Planning and Care: Research Scan
- Addressing Inequities in End-of-Life Planning and Care: Advancing Equity at Life’s End Summit Report
- COVID-19 Impact on Underserved Communities
Webinars and Opeds
- Death, Dignity and Disabilities
- Engaging Communities of Color: Ensuring All Americans are Prepared for the Inevitable End
- Inglewood Today: COVID-19 Crisis Highlights Ways to Combat Health Disparities for People of Color
- Making Your Wishes Known: Living Your Values by Planning Ahead
- People of Color Need Better Access to All End-of-Life Care Options
- Hospice is about Living, not Dying by Missy Moore
- A Legacy worth Leaving by Avery Ross
1 https://www.liebertpub.com/doi/abs/10.1089/jpm.2018.0436; ; https://www.sciencedirect.com/science/article/pii/S0885392418300277#bib6.
2 https://pubmed.ncbi.nlm.nih.gov/32767722/; https://onlinelibrary.wiley.com/doi/full/10.1002/hast.1135; https://proceedings.med.ucla.edu/wp-content/uploads/2020/06/Wells-A200421LW-rko-Wells-Lindsay-M.D.-BLM-formatted.pdf.
4 Cindy L. Cain, et al., Culture and Palliative Care: Preferences, Communication, Meaning, and Mutual Decision Making, 55(5) J Pain Symptom and Management 1408-1419 (2018) https://www.sciencedirect.com/science/article/pii/S0885392418300277#bib6
5 Cindy L. Cain, et al., Culture and Palliative Care: Preferences, Communication, Meaning, and Mutual Decision Making, 55(5) J Pain Symptom and Management 1408-1419 (2018) https://www.sciencedirect.com/science/article/pii/S0885392418300277#bib6


