Kate shared her story in June 2020.
After six months of unexplained symptoms and a dozen or more medical tests and scans, my dad was diagnosed with amyotrophic lateral sclerosis (ALS) – a neurodegenerative, terminal disease – in September of 2013. Typically, people survive anywhere between 18 months and 5 years after diagnosis as their body slowly abandons them. ALS essentially causes the brain to stop talking to different body parts, ultimately significantly reducing functionality in muscles.
ALS is largely considered by doctors to be one of the worst diagnoses one can receive. It is 100% terminal and there are few treatments to improve quality of life. The day my dad was diagnosed, I rushed to his side. After the rest of our family went to bed, we stayed up talking and I promised him I would find a way to be in control of his death.
Living in Virginia, medical aid in dying wasn’t an option, so he – as he was just handed a death sentence – was concerned for me, appreciating the offer, but not wanting me to get in trouble because of him. I assured him I wouldn’t jeopardize my safety, that aid in dying was possible in other states, that I wouldn’t sit by and watch him suffer more than he was willing – he would die on his own terms. The next morning, my dad quietly told me it was the first night he slept in weeks. He said, when this terrible disease robbed him of all control over his body, knowing he would have some semblance of control over his end-of-life experience brought him peace.
Dad’s health deteriorated rapidly. Within three months of being diagnosed, he was in a wheelchair and by spring, he was fully paralyzed and suffering from oxygen depletion. He had a permanent CPAP placed, which covered his nose and mouth, leaving Dad having to choose between breathing and eating or breathing and talking. He was truly miserable.
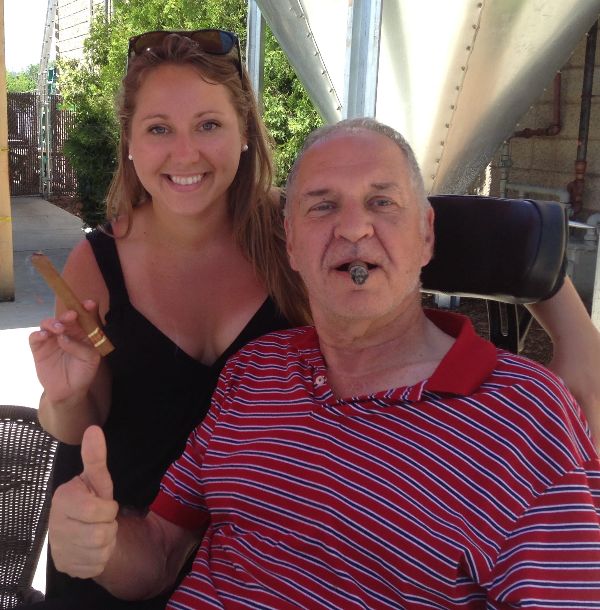
A few months later, a respiratory therapist told us about the nasal pillow, a device which fits directly into the nostrils to deliver pressurized air without restricting the use of his mouth. Dad regained – in his words – a good quality of life and could once again enjoy things he loved before his diagnosis. Although he missed playing the clarinet – he was a lifelong, prolific musician – he could now freely engage in intellectual and political discussions and relish in good food and drinks at local breweries and wineries. ALS did not slow him down, but the thought of suffering an agonizing and prolonged death weighed heavily on him.
Fortunately, we never had to discuss again the option of moving to another state. Dad died at the age of 67 in his sleep on March 9, 2015. He was a huge proponent of quality of life and autonomy. He believed no one should be made to suffer unnecessarily and a person’s end-of-life options should not be limited due to living in the wrong zip code.
I strongly believe the best way to honor those whose lives are cut far too short is to respect their wishes to end suffering and pass in peace. Not everyone has the ability to relocate, particularly when plagued with a disease requiring tremendous care and expenses. No terminally ill person should have to move to another state to achieve peace of mind regarding their final days. What little time and energy they have left should be spent with the ones they love, not riddled with stress, fear, and anxiety.