Status of End-of-Life Legislation
The Illinois End-of-Life Options for Terminally Ill Patients Act (SB 3499), that would authorize medical aid in dying in Illinois, was introduced in the Senate on February 8, 2024 by Assistant Majority Leader Linda Holmes (D 42). The legislation is summarized here.
The majority of Illinoisans support medical aid in dying. In a 2023 poll, 71% of likely Illinois Voters supported this compassionate legislation. The majority of Illinois physicians also support this option with the key safeguards in the legislation
Survey of Illinois Physicians’ Attitudes Toward Medical Aid in Dying as an End-of-Life Option
Illinois Legislative Campaign Overview
The Compassion & Choices Action Network Illinois team and the ACLU of Illinois are partnering in the Illinois End-of-Life Options Coalition to advocate for the end-of-life care option of medical aid in dying for qualified terminally ill Illinoisans. If you would like to get involved in this movement, please sign up here.
Polling
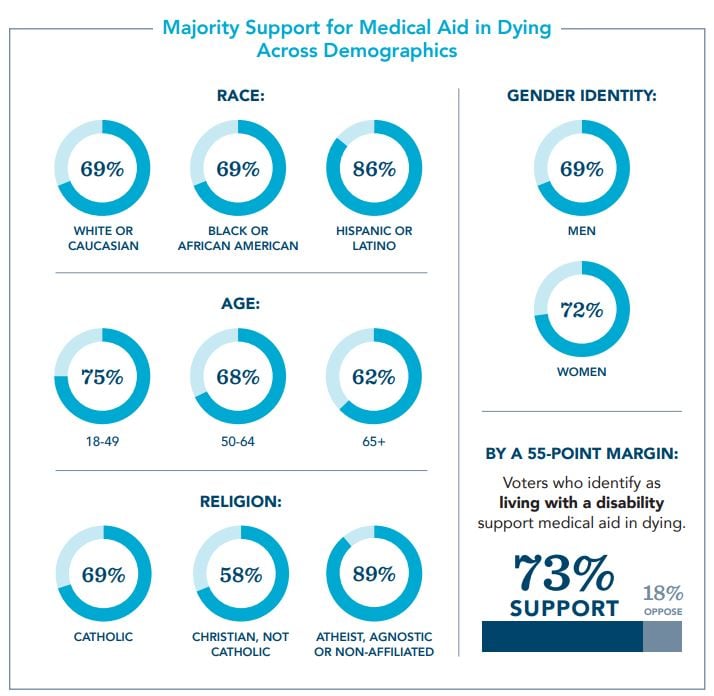
Legislation to allow medical aid in dying, an option for mentally capable, terminally ill adults to peacefully end unbearable suffering, is supported by a wide majority of Illinois voters, regardless of political affiliation, disability, race, gender identity, age or religion.
Hear from Illinoisan Deb Robertson
Nilsa Centeno is the mother of the late Miguel Carrasquillo, a Chicago chef who died in his native Puerto Rico in 2016 of brain cancer while advocating for medical aid in dying.
Take Action
- Contact Your Lawmakers: Though we do not yet have a bill in Illinois, let your lawmakers know your position on medical aid in dying and ask them to be supportive when there is a bill.
- Check out our Virtual Advocacy Guide: Find out how to virtually advocate for end-of-life care in the most effective way.
- Watch: In June, 2021, Compassion & Choices Midwest Regional Advocacy & Outreach Manager Amy Sherman appeared on the Women Over 70 podcast to discuss end-of-life planning and care. Check it out on YouTube.
- Share your Story:: Stories have the power to change minds. Submit your experience with end-of-life issues, and we’ll help you get your story out.
- Join an existing Action Team in Illinois or start a new one.
- Join Compassion & Choices Illinois
- Sign up to volunteer: Join others to help educate others about issues to improve end-of-life care and expand end-of-life choice.
- Attend an Event: Meet others while learning more about end of life options.
- Schedule an event: We’ll help you host an event to educate others and encourage them to take action.
- Find us on Facebook.
- Learn about medical aid in dying: This summary provides you with everything you need to know about medical aid in dying.
Tools and Resources

 For Patients Access the Illinois Advance Directive
For Patients Access the Illinois Advance Directive
 End-of-Life Planning Use our step-by-step guide to chart your journey.
End-of-Life Planning Use our step-by-step guide to chart your journey.
 Los recursos en Español Los recursos en Español.
Los recursos en Español Los recursos en Español.
 COVID-19 Toolkit Get answers to your questions about COVID-19
and end of life care.
COVID-19 Toolkit Get answers to your questions about COVID-19
and end of life care.
 Resources for Providers Find resources tailored to the needs of healthcare providers.
Resources for Providers Find resources tailored to the needs of healthcare providers.



